|
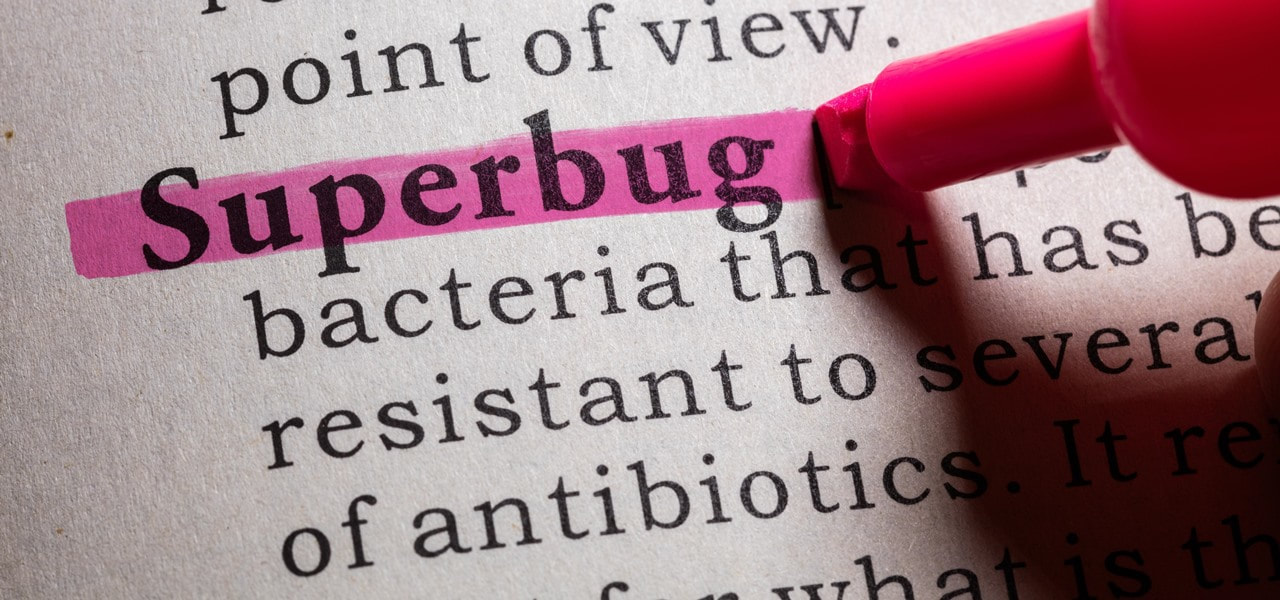
Leaving the doctor's office with a script for antibiotics which might not be needed is contributing to the global problem of resistance to antibiotics. Antibiotic resistance happens when bacteria change or mutate to protect themselves from an antibiotic. Mutated bacteria can also pass their genes to other bacteria, forming a new antibiotic resistant ‘strain’ of that bacteria. (1) A 5 YEAR Australian report released in 2017 found that antibiotics are prescribed for acute respiratory infections at rates of 4–9 times higher than those recommended by our national clinical guidelines. (2) If Australian doctors were to start prescribing antibiotics along these national guidelines, the number of pills handed out for some conditions would fall by nearly 90 per cent. Also in 2017, WHO (World Health Organisation) released a report confirming that the world is running out of antibiotics. (3) This report found that most of the antibiotics currently in use are modifications of existing antibiotics and are only short-term solutions. The report also found very few potential treatment options for antibiotic resistant infections identified as posing the greatest threat to human health, such as drug-resistant tuberculosis which kills around 250 000 people every year. In addition, WHO identified 12 classes of priority pathogens – some of which cause common infections such as pneumonia or urinary tract infections – that are increasingly resistant to existing antibiotics and urgently in need of new treatments. Antibiotics have been in use for 70 years and undoubtedly have saved millions of lives. However, during the last 50 years just one antibiotic that works in a new way has been discovered and developed for use in humans. One! (4) The time it takes for bacteria to become resistant to antibiotics is getting shorter. We NEED to change the way we are using antibiotics. NPS medicine wise is an independent Australian, not-for-profit and evidence-based organisation that works to improve the way health technologies, medicines and medical tests are prescribed and used. Australians are over-using antibiotics. Australia is the eighth highest user of antibiotics out of 28 European countries. In 2015, Australian doctors prescribed more than 30 million antibiotic scripts through the Pharmaceutical Benefits Scheme. Antibiotic resistance is already impacting our health. Antibiotic-resistant infections are not just seen in hospitals, agriculture or countries overseas, and they are not a future problem. Antibiotic resistance already affects individuals in Australian communities. Infection with antibiotic-resistant bacteria means longer stays in hospital and a higher death rate. If you have an infection caused by bacteria resistant to antibiotics you are more likely to die from that infection. In Australia, the prevalence of multi-resistant bacteria (‘superbugs’) is increasing with more & more patients getting infections which are resistant to multiple antibiotics. Examples of superbugs in our communities which have already developed resistance to a number of antibiotics include strains of Escherichia coli (E coli) that cause many urinary tract infections and ‘Golden staph’, a common cause of skin infections. Failure of the last-resort antibiotic treatment for the sexually transmitted infection gonorrhoea is now also occurring in Australia. (5) What can we do? According to the World Health Organisation, antibiotic resistance is one of the biggest threats to human health today. What you do as an individual has a real impact on antibiotic resistance. This is a problem we can have control over. Actions we take as individuals can make a difference, because the more antibiotics are used, the more chances bacteria have to become resistant to them which is already making bacterial infections much harder to treat. Again, (E coli) that causes many urinary tract infections and Golden staph, a common cause of skin infections. There are five things you can pledge to do to reduce antibiotic resistance:
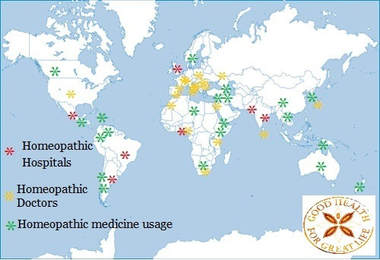
Also, I encourage you to think about the origin of the foods you are buying. Feed your family, certified organic where possible which in Australia means no antibiotics are used to grow the fruit, veg and meat products. Lessening the consumption of antibiotics. Green snot doesn’t mean you need antibiotics Coloured mucous or phlegm isn’t always a sign of a bacterial infection, and that also goes for other symptoms including cough, sore throat, earaches and fever. While some people with these symptoms will need antibiotics, most people won’t and will get better without antibiotics. Green or yellow coloured snot can in fact be a sign that your immune system is fighting the infection, and not that the illness is getting worse. (6) Don’t share antibiotics with another person. This is important because the type of antibiotic may not be targeted to the bacteria causing their particular infection. Antibiotic resistance can have personal consequences for you, your family and the community. Antibiotic-resistant bacteria can persist in your body for as long as 12 months and may be passed on to family members or others in the community. Can complimentary medicine can play a role in reducing antibiotic resistance? Researchers led by the University of Bristol collected data from over 7,000 GP clinics and compared it with nine clinics where GPs integrated complimentary medicine in their daily practice. Analysis showed that practices which employed GPs with additional training in complementary medicine, such as homeopathy, prescribed 22% fewer antibiotics. (7) A common misconception in that there is no evidence for homeopathic medicine – this is just not true! It’s true to say that there are not a huge number of studies, but some evidence is very different from no evidence. By the end of 2014, 189 randomised controlled trials of homeopathy on 100 different medical conditions had been published in peer-reviewed journals. Of these, 104 papers were placebo-controlled and were eligible for detailed review. (8),(9) Homeopaths acknowledge that the body of evidence for homeopathic medicine is small but growing and much more research needs to happen. Homeopathic medicine has been in use for over 200 years without a single microbe becoming resistant to it. Why? Because homeopathic medicines aim to strengthen the person against the bacteria or virus; a stronger person being more resilient to recurring infection. Homeopathic medicine is legally recognized as a distinct system of medicine in 42 countries. Argentina, Brazil, England, Ghana, India, Mexico, Pakistan and Scotland all have Homeopathic hospitals integrated into their Healthcare systems. (10) It is estimated that there are over 350,000 qualified medical doctors prescribing Homeopathic medicine worldwide and 200,000,000 people using Homeopathic medicine. Homeopathic medicine is not a one size fits all over the counter prescription. It needs to be skillfully prescribed for the symptoms the person is suffering not for the name of the disease or condition. HRH The Prince of Wales's speech to the Global Leaders Conference on Antimicrobial Resistance. An excerpt...''Ladies and Gentlemen, I really am delighted to have had a brief opportunity to meet many of you just now and would like to commend you on your strenuous efforts – at long last – to address the grave threats to health posed by antimicrobial resistance. As some of you may possibly be aware – maybe not - this issue has been of long standing and acute concern to quite a few people, including myself (in fact, it was one of the reasons I converted my farming operation to an organic – or agro-ecological – system over thirty years ago, and why, incidentally, we have been successfully using homeopathic – yes homeopathic - treatments for my cattle and sheep as part of a programme to reduce the use of antibiotics). So, I take great heart from the fact that Ministers, officials and scientists of such eminence and from so many countries are putting their collective minds to the development of a concerted course of action.'' (11) REFERENCES
1. https://www.nps.org.au/medical-info/consumer-info/antibiotic-resistance-the-facts?c=bacteria-become-resistant-to-antibiotics-not-your-body-9e5685a3 2.https://www.mja.com.au/journal/2017/207/2/antibiotics-acute-respiratory-infections-general-practice-comparison-prescribing 3. http://www.who.int/mediacentre/news/releases/2017/running-out-antibiotics/en/ 4.https://www.nps.org.au/medical-info/consumer-info/antibiotic-resistance-the-facts?c=the-drug-pipeline-for-antibiotics-is-drying-up-d81a6b23 5.https://www.nps.org.au/medical-info/consumer-info/antibiotic-resistance-the-facts?c=antibiotic-resistance-is-already-impacting-our-health-37c45430 6.https://www.nps.org.au/medical-info/consumer-info/antibiotic-resistance-the-facts?c=green-snot-doesn-t-mean-you-need-antibiotics-f91ee557 7.http://bmjopen.bmj.com/content/8/3/e020488 8.facultyofhomeopathy.org/research/ 9.https://www.hri-research.org/resources/homeopathy-faqs/there-is-no-scientific-evidence-homeopathy-works/ 10. drnancymalik.wordpress.com/article/status-of-homeopathy/ 11.www.princeofwales.gov.uk/speech/hrh-prince-waless-speech-global-leaders-conference-antimicrobial-resistance |
AuthorSkilled in unravelling complex patterns of ill health, Sarah Penrose is a qualified, registered and endorsed natural health professional specializing in homeopathic medicine. Archives
December 2022
Categories |



 RSS Feed
RSS Feed



